As COVID cases rise in Ontario schools, could an extended school break help slow the pandemic?
Before her kids go on Christmas break, Lindsay Matheson is going to make sure they bring their indoor shoes home from school.
With cases surging across the province, the weather getting worse — and a holiday season that will undoubtedly find families mixing, mingling and flouting the rules of social distancing — Matheson can’t imagine school will resume as per normal come January.
“This feels exactly like what happened in March,” said Matheson, a Toronto teacher and mom of three, of how students believed they’d return to school at some point after spring break, but never did.

“I kind of expect the same thing is going to happen now. So I’m going to learn from experience.”
While parents and teachers of elementary and secondary schools may be anticipating, and even planning for, a post-vacation lockdown, there has been no official word on an extended break — or a return-to-school strategy.
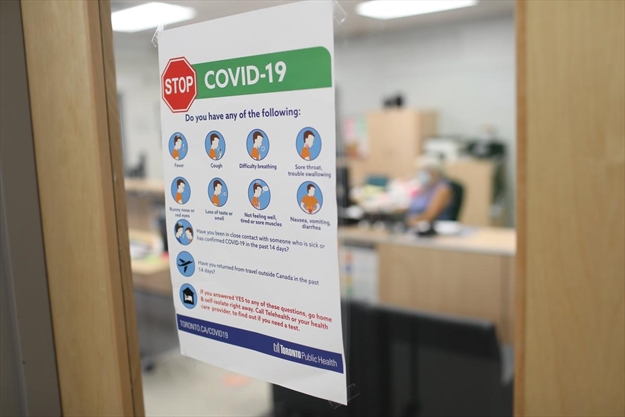
Toronto Public Health continues to push safety protocols already in place. School boards keep urging families to stay in their bubbles. And while universities in Ontario as well as other provinces, including Alberta, have long ago announced extended winter breaks or pivots to online learning, Ontario’s education minister remains mum on the issue.
In an emailed statement to the Star, spokesperson Caitlin Clark said that throughout the pandemic, the ministry has been guided by the chief medical officer of health, “the most senior public health authority in this province,” and “while some teacher unions have called for the closure of schools this fall, we believe schools should safely remain open.”
From Nov. 23, through the first week in December, the total number of school-related COVID cases, both active and resolved, jumped 48 per cent, according to epidemiologist Ahmed Al-Jaishi, who tracks cases across the province and in Ontario’s schools. In those 14 days alone, his data shows, active COVID cases increased by 35 per cent, leaping from 1,331 confirmed cases in 757 schools on Nov. 23 to 1,803 active cases in 947 schools Tuesday. (Those rose to 1,866 cases in 969 schools Wednesday.)
Since September, Al-Jaishi’s data shows, 43 per cent of Ontario schools have had at least one case of COVID and right now, about 20 per cent of schools have an active case. On Tuesday, Marc Garneau C.I. became the third TDSB school to be shut down.
Peter Juni, scientific director of the province’s COVID-19 Science Advisory Table, told the Star that extending the winter break by a week or so is not a bad idea, if we all are disciplined. But if we continue to socialize as a society, he said, “then it will probably not help much or at all.”
Juni, also a professor of medicine and epidemiology at the University of Toronto’s Temerty Faculty of Medicine, said that right now it is important for the government to come up with a decision — to extend the break or not — and give people enough time to plan. Whatever the decision, he said, it is also imperative to focus on communities where transmission is high and take additional measures in those schools.
Leslie Wolfe, who heads the Toronto local of the Ontario Secondary School Teachers’ Federation, is calling on the province to announce an extended break, saying they should already have done so out of “an abundance of caution.” And to give teachers time to prepare. Even though teachers have been told since Day 1 to be ready at any time to pivot to online learning, doing it well takes planning and preparation.
“There needs to be enough notice for teachers to do the detailed kind of planning they would do,” she said.
On Wednesday, the group urged the province, Toronto Public Health and the Toronto District School Board in to close schools for at least two weeks after the break (with online lessons) and fund asymptomatic testing at all TDSB schools.
Taking the extra time after the break may be particularly important, she said, because kids may transmit the virus asymptomatically. The extra time following Christmas and New Year’s may at least allow for parents to see if symptoms develop.
A Sept. 21 article in the Canadian Medical Association Journal titled “Have we misjudged the role of children in spreading COVID-19?” explores whether kids play a larger role in transmission of the virus that initially suspected. The picture of whether and how young kids are involved in the spread is “confusing,” the article says, because of blind spots in the early research as well as potential bias.
Research showing that kids have fewer antibodies than adults may be misleading, the article says, because they were done when schools were closed and transmission among children was likely low. By the same token, the article says, the murky research has made it difficult to tease apart whether or how school closures have affected transmission rates. Or how many kids are asymptomatic.
Other studies in the last three months have
While Jennifer Brown, president of Elementary Teachers of Toronto, said she feels it’s important for kids to get back to school as soon as possible, she says it needs to be done in the safest possible way. For her, that means reducing class sizes to where both students and teachers can maintain a proper social distance as well as making sure each child has a proper mask and is taught in a well ventilated building.
There are school buildings that are in need of repair, she said. “Many parents would prefer for their kids to be in school,” she said, “if they were confident in the safety measures put in place.”
Even about a month ago, Matheson said it seemed for a bit that schools might escape the rise in cases. But over the last couple of weeks, she said, there have been cases at the school her daughters attend — and at the school where she teaches. And now, she said, things feels like they are closing in. She and her family plan to keep a low profile over the holidays.
But will everyone else? Matheson said she is nervous about the return to school, and said she’s angry at the government for “making this feel very last-minute.”
Michele Henry is a Toronto-based reporter for the Star, writing health and education stories. Follow her on Twitter: